By Macall Leslie Salewon, MPH, Epidemiologist
Background
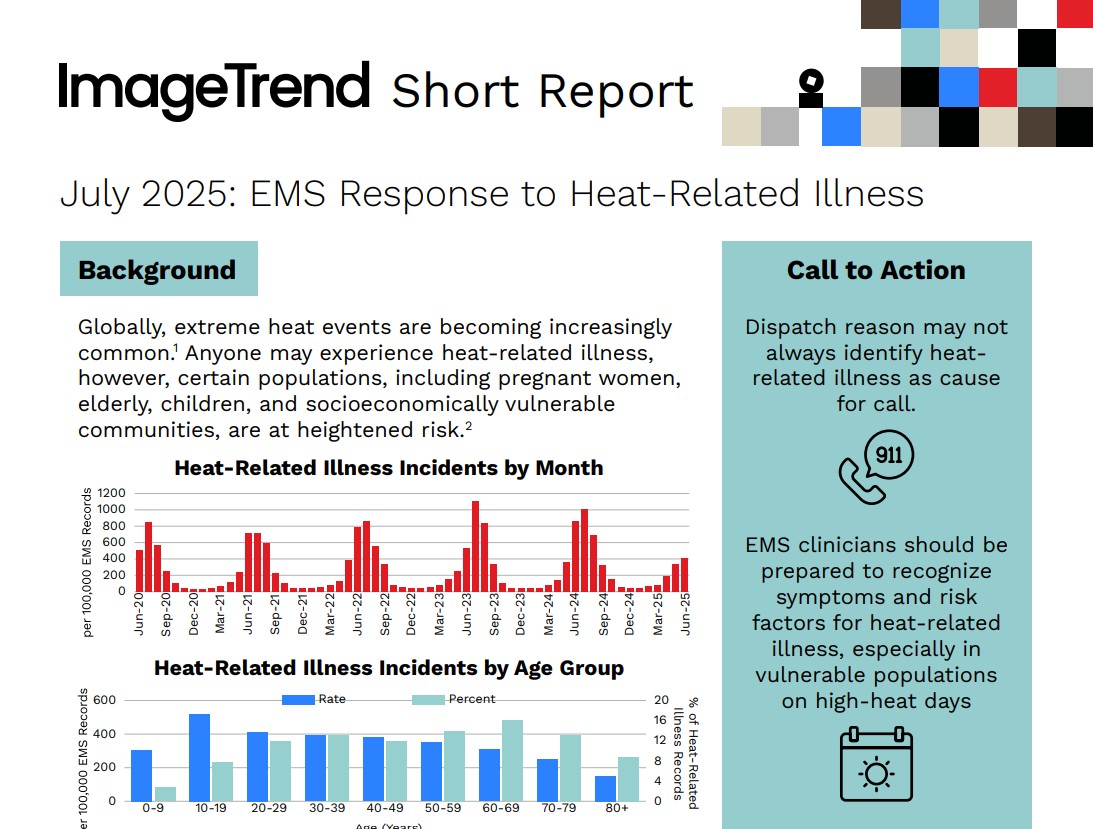
Extreme heat events are growing in both frequency and intensity across the globe.¹ In the United States, heat is the leading causes of weather-related deaths,¹ and record-breaking temperatures in 2023 contributed to almost 120,000 emergency department visits for heat-related illness (HRI).²
While anyone can be affected, certain populations—including elderly individuals, children, pregnant women, and residents of socioeconomically disadvantaged communities—are disproportionately at risk.³
This report analyzes EMS response patterns to heat-related illness using biospatial® data, with insights into patient demographics, incident locations, and severity levels to better guide prevention and preparedness efforts.
Key Findings
Who Is Affected?
- 61% of heat-related EMS responses involved male patients.
- Adolescents aged 10–19 showed a unique risk profile, with 24% of incidents occurring at athletic or recreation areas—more than double the overall rate of 11%.
- Older adults aged 80+ were significantly more likely to experience heat illness at home, with 65% of cases occurring at a private residence (compared to 47% across all age groups).
How Severe Are the Cases?
- 68% of heat-related incidents resulted in patient treatment and/or transport.
- 25% of patients were categorized as having “emergent” acuity upon EMS arrival.
- 3% were considered “critical”, highlighting the potential for rapid deterioration, particularly among high-risk groups.
Call to Action
While 9-1-1 dispatch reasons may not always identify heat as the underlying cause, EMS personnel must remain vigilant in recognizing symptoms of heat-related illness—especially during periods of extreme temperatures.
To improve outcomes and reduce preventable illness, EMS agencies and community health partners should:
- Enhance frontline training to improve symptom recognition and triage of heat-related illness across diverse populations.
- Proactively identify high-risk communities, such as areas with a high density of elderly residents or low access to air conditioning.
- Coordinate community wellness checks, especially during heatwaves, for homebound seniors and other vulnerable individuals.
- Partner with youth sports and recreation programs to promote hydration, heat safety awareness, and rapid response planning.
- Support access to local cooling centers through public messaging, transportation coordination, and targeted outreach during heat advisories.
For EMS clinicians and community partners looking to strengthen their understanding of heat-related illness, the following resources offer practical guidance on recognition, assessment, and response:
- Hyperthermia: EMS Assessment and Management – EMS1
- Managing Heat-Related Stress in EMS – Federal Healthcare Resilience Work Group (PDF)
These tools can support frontline readiness and improve patient outcomes during extreme heat events.
About the Data
This analysis was conducted using biospatial® data by ImageTrend, leveraging the Heat-related Illness Syndrome classification to examine EMS responses across the U.S. This encompassed 85,323,597 9-1-1 EMS activations in over 40 states.
biospatial® data includes real-time EMS activations and trends, offering a detailed look at emerging threats and public health risks.
About biospatial® by ImageTrend
biospatial® combines EMS electronic patient care reports (ePCR) from our growing network of thousands of EMS providers with other electronic healthcare data sources using proprietary artificial intelligence (AI) to support the missions of public sector and commercial healthcare entities.
To explore participation or propose a research topic, contact our Clinical & Research Services team.
Correspondence
- ClinicalResearch@ImageTrend.com
- Clinical & Research Services ImageTrend, Inc. 1305 Corporate Center Dr, Eagan, MN 55121
Citations
- U.S. Environmental Protection Agency (EPA). Extreme Heat. https://www.epa.gov/climatechange-science/extreme-heat#impacts. Accessed June 18, 2025.
- Centers for Disease Control and Prevention (CDC). Heat-Related Emergency Department Visits — United States, May–September 2023. Morbidity and Mortality Weekly Report. https://www.cdc.gov/mmwr/volumes/73/wr/mm7315a1.htm#:~:text=Characteristics%20of%20HRI%20ED%20Visits,several%20HHS%20regions%20in%202023. Accessed July 2, 2025
- Centers for Disease Control and Prevention (CDC). People at Increased Risk for Heat-Related Illness. https://www.cdc.gov/heat-health/risk-factors/index.html. Accessed June 18, 2025.
Related Resources
Tomorrow Won’t Look Like Today. Prepare for What’s Next.
See the bigger picture and confidently face the challenges ahead with our industry-leading solutions.