At Montgomery County Hospital District (MCHD) in Texas, data is more than just numbers—it’s the backbone of better documentation, informed decision-making, and improved patient care. As an EMS Data Analyst, Michael Wells wears many hats, working with clinical and operational teams to transform data from CAD, ImageTrend Elite, Data Mart, and even billing systems (all integrated through ImageTrend’s all-in-one platform) into actionable insights.
From closing the loop between EMS and hospitals to reducing documentation time for crews in the field, MCHD has built a culture where technology supports people, not the other way around. Through hospital integration, configurable Validation Rules, and ongoing feedback from providers, Wells and his team are proving that when data quality improves, so does the care patients receive.
You can scroll down to watch the full video from Michael’s recent Connect25 interview, where he shares how this approach came together.
Closing the Loop Between EMS and Hospitals
“The hospital outcome data is crucial for our continuous quality improvement process and ensuring that our field providers really are working at the top of their clinical game,” Wells said.
Those outcomes are possible thanks to relationships with hospital partners. “Once you have the buy-in from the hospital and buy-in from your EMS leadership, then it just comes down to working out the technology, which is the easy part.”
This connection doesn’t just support clinical review; it also impacts provider well-being:
- Reducing traumatic stress and chronic stress by providing “loop closure.”
- Delivering “the gold standard” of what was actually wrong with the patient for clinical education.
Hospital data, seamlessly connected through their all-in-one platform approach, also powers MCHD’s research efforts:
- Comparing the accuracy of the telephone stroke diagnostic tool with field activations.
- Validating results against hospital outcome data to determine whether the patient actually had a stroke.
“We wouldn’t be able to do what we do without Data Mart,” Wells added. “Having the very granular access to every single data point in our system…really has made it possible for us to do what we do today.”
Designing Workflows That Work for Crews
“There are really two core values that me and my team apply to how we manage our software systems,” Wells said:
- Make the path of least resistance the correct way – so human nature works for you instead of against you.
- Cognitive offloading – use technology to handle repetitive details, letting providers focus on patient care.
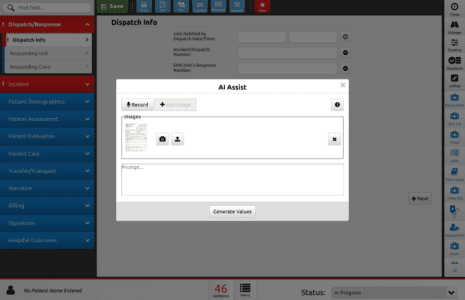
This approach drives how MCHD builds Validation Rules in ImageTrend Elite. “Whether that’s calculating medication dosages or using Validation Rules so crews don’t have to remember ‘when I transport to this hospital, this has to be filled out differently,’ we can use the technology to guide them through that, so it’s just one less thing for them to focus on.”
Improving Data Quality One Rule at a Time
When asked to share a specific rule or configuration that improved behavior or data quality, Wells said it’s difficult to choose just one.
“It’s hard to narrow it down to one particular rule,” he said. “We have kind of a continuous improvement idea when it comes to our Validation Rules. Any issue that comes up, whether it’s in clinical review or operational review, if it’s something that we can solve with a validation rule, we’ll make that change. We’re making changes almost every week to continue to hone those validation rules.”
One example that’s made a significant impact involves capturing hospital encounter numbers. To address common errors and inconsistencies, MCHD’s validation rules now:
- Require each hospital’s number to match its correct length and prefix.
- Flag placeholder entries like 99999 or 11111.
- Prompt crews to explain when the number can’t be obtained, such as during delayed hospital registration.
This approach makes “the path of least resistance…to just do it correctly,” while still accounting for situations where the number isn’t available.
“The old saying of garbage in, garbage out really does apply…Everything that we do to improve the data quality directly benefits the patients in our community,” he explained.
Building Trust and Feedback Loops
“When we first implemented…the biggest complaint was, well, I was done so quickly, it doesn’t feel like I actually finished my report,” Wells said.
Early feedback included:
- 10–15 minutes saved per chart.
- A more streamlined, easier-to-use workflow.
As the system matured, the culture shifted:
- Field providers began bringing suggestions forward.
- Small fixes often took only minutes, building trust and provider buy-in.
- “The entire organization is working to improve [the ePCR], which then improves data quality and then improves the clinical care that we’re able to provide to our patients.”
Advice for Other Agencies
“If you don’t have a clinical background…you have to get out in the field, go do some ride-alongs with your people,” Wells advised.
If you do have a clinical background:
- Stay connected to provider workflows.
- “Build the relationships with your crew members and always be open to feedback.”
- Remember: “There is something that we can learn from everyone.”
His final takeaway: “Give them the grace and patience to do what they do best…the clinical care…so that we are keeping our patients the center of everything that we do.”
Technology That Supports a Data-Driven Culture
With ImageTrend’s all-in-one platform, including Elite and Data Mart, MCHD can design Validation Rules, integrate hospital outcomes, and analyze data in near real-time, fueling their quality improvement, research, and provider support efforts.
As Wells’ experience shows, the right tools + the right culture transform documentation from a task into a driver of better care.
Watch the Full Interview
Hear Michael Wells share more about how MCHD uses technology, data, and collaboration to strengthen EMS documentation and patient care.
Optional Pre-Title H3 – Basic Content on White
Paragraph Text – Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat.