When seconds matter and specialized care is needed, how do EMS teams decide between air and ground transport?
A new multi-state research initiative powered by ImageTrend’s Elite platform offers fresh insight into this critical question, shedding light on how patient acuity, geography, and resource availability intersect in the interfacility transfer (IFT) process.
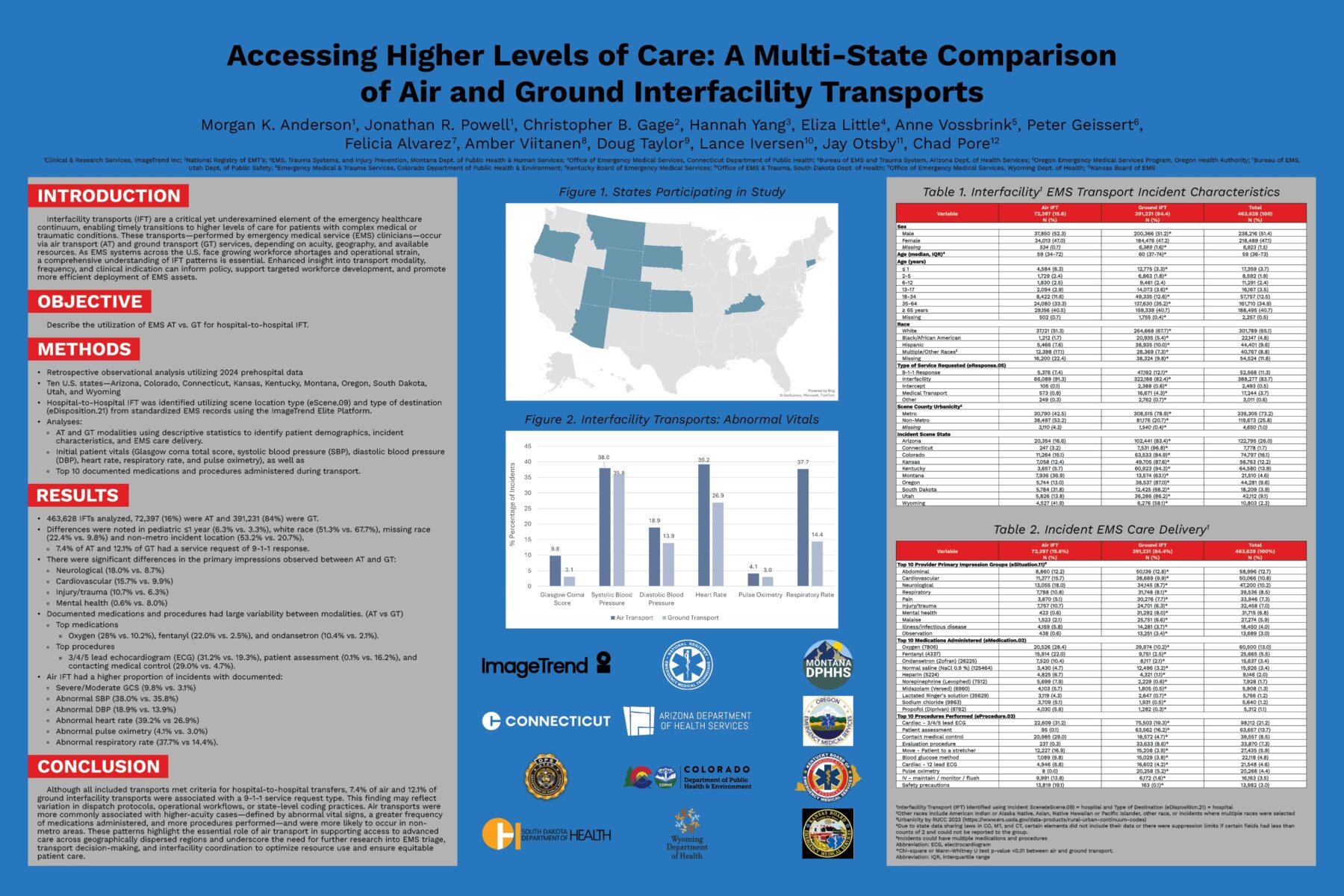
Conducted in collaboration with 10 U.S. state EMS offices, this first-of-its-kind study analyzes over 460,000 hospital-to-hospital EMS transports across air and ground modalities. The findings not only highlight the vital role EMS plays in bridging care gaps but also uncover new opportunities for selective resource deployment, cost-efficiency, and equitable access to care.
Why Interfacility Transports Deserve More Attention
IFTs—transfers from one hospital to another—are a vital yet often overlooked component of the emergency care continuum. These incidents often involve high-acuity patients in need of specialized treatment not available at the sending facility: NICU services, trauma or burn care, advanced cardiac intervention, and more.
As EMS agencies across the U.S. face mounting operational pressures—from workforce shortages to rising service costs—understanding when and how IFTs are performed is essential to managing resources efficiently and ensuring the right care reaches the right patients at the right time.
What the Interfacility Transports Data Tells Us
Using standardized EMS records captured via ImageTrend Elite, our researchers examined 463,628 IFTs across 10 states occurring in 2024. Of these:
- 84% were ground transports
- 16% were air transports
Key findings reveal:
Higher Acuity = Higher Altitude. Patients transported by air were far more likely to present with severe clinical indicators, including abnormal heart rate, respiratory rate, systolic/diastolic blood pressure, and Glasgow Coma Score.
Geography Drives Modality. Over 53% of air IFTs originated in non-metro areas, compared to just 21% of ground transports. In rural regions, air transport—whether by helicopter or fixed-wing aircraft—often provides the fastest, and sometimes only, connection to higher-level care. These findings highlight the critical role of air resources in bridging geographic gaps where quality of care, distance, terrain, or limited local hospital capabilities make timely ground transport impractical.
Neonatal Need for Speed Leads to Pediatric Spikes. A notable increase in air transports for infants under 1 year old was observed—suggesting that neonatal patients are often moved urgently to facilities with NICU capabilities not available at the originating hospital.
Critical vs. Clinical Diagnoses Diverge. Air transports were more likely to involve neurological (18%), cardiovascular (15.7%), and injury/trauma (10.7%) impressions. Ground transports, by contrast, had higher rates of mental health (8%) and malaise-related assessments (6.6%).
System-Wide Interfacility Transports Implications
This study doesn’t just offer data points—it brings clarity to complex questions about how EMS resources are deployed, especially in critical interfacility scenarios.
While air transports are often necessary for urgent or rural cases, their significantly higher cost raises important questions. As ImageTrend Research Manager Morgan K. Anderson explained, “This research helps agencies ask, ‘Are we using air assets where they’re truly needed—or are there patterns of overutilization that need addressing?’”
Geography emerged as a consistent factor. Non-metro regions relied heavily on air transport, largely due to time-sensitive needs and the absence of specialty care services nearby. In many cases, air transport wasn’t just faster—it was the only viable option for reaching trauma centers, NICUs, or advanced cardiac care units.
This research also uncovered critical insights into gaps in pediatric, neurological, cardiovascular, and trauma-based infrastructure. A notable spike in air transports for infants under 1 year old suggests a lack of NICU services at smaller hospitals—particularly in rural areas. This trend may also reflect a broader issue: rural hospital closures across the U.S., many of which include obstetric (OB) services, further limiting access to specialized care for mothers and newborns.
Across all age groups, air transports were significantly more likely to involve neurological (18%), cardiovascular (15.7%), and injury/trauma (10.7%) impressions—conditions that often require time-sensitive, specialized interventions. Further research could help determine whether these patients were specifically being transported to trauma-designated hospitals or other specialty centers equipped to handle complex emergencies. These patterns underscore the need for better cross-system coordination and real-time data access between EMS and hospitals.
Ultimately, this research gives state EMS offices and hospital networks a foundation for evaluating resource allocation, advocating for infrastructure investments, and designing more strategic care transitions, especially for underserved populations.
The ImageTrend Advantage
This research was made possible by comprehensive, high-quality EMS data collected and standardized through ImageTrend Elite—our all-in-one ePCR and data management solution trusted nationwide.
If you’re looking to deepen your visibility into interfacility transports and improve decision-making, additional ImageTrend solutions can help:
- Health Information Hub (HIH): Real-time, bidirectional data exchange between EMS and hospitals for better care coordination.
- Continuum: Dashboards and alerts that help agencies monitor performance, resource usage, and care outcomes in real time.
- Collaborate: De-identified data across agencies and regions to uncover macro-level insights and emerging trends.
This research was presented at the 2025 NASEMSO Annual Meeting, May 12–16 in Grand Rapids, MI.
Optional Pre-Title H3 – Basic Content on White
Paragraph Text – Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat.